| Katherine Roberts, University of Manchester | The UKAHN Bulletin |
| Volume 10 (1) 2022 | |

In a 1943 article published in the Nursing Times, the Matron-in-Chief of the Queen Alexandra’s Imperial Military Nursing Service, Dame Katherine Jones, recounted her experience of traveling to North Africa in order to see service members on active duty. ‘It is grim,’ she proudly reported, but ‘they are busy and nothing matters when they have their nursing work to do’.[1] In her article, Dame Katherine presented an image of a nursing force that readily dismissed the physical difficulties created by their working environment and who remained unaffected by the emotional impact of negative sensory experiences.
This article aims to interrogate the image put forward by Dame Katherine and asks how the popular construction of the nurse’s body contrasted with the reality of her embodied experience. In order to illustrate the connection between the body and emotions, the article begins with a discussion of the concept of embodiment. It moves on to address how an individual’s social world influences not only how they perceive their embodied experiences, but also the way that they narrate those experiences to others and then presents an overview of the expectations surrounding bodily presentation that structured British nurses’ social world during the Second World War. Drawing on these concepts, the article uses textual analysis to examine the letters and diaries written by seven active-duty Queen Alexandra’s Imperial Military Nursing Service Sisters (QA’s) and discusses the ways in which these women characterised their embodied experience. The QA’s under consideration are Sisters Joyce Ffoulkes Parry, Nell Jarrett, Vera Jones, Helen Luker, Agnes Morgan, Mary Morris, and Betty Murgatroyd.
Embodiment: integrating the body, the mind, and the social world
The notion of embodiment argues that there is no division between an individual’s body and their mind. An embodied individual exists as a unified being in their mental and physical experiences; philosopher Maurice Merleau-Ponty argued that ‘bodily experience’ was the ‘primary source of perception’ through which an individual came to know their world.[2] Therefore, an individual’s physical characteristics and bodily processes ‘shape their experiences and the way they are present in the world’.[3] Professor Rachel Cooper draws on this theory in order to argue for the influence of an individual’s physical environment on their emotional state. Cooper argues that the sensory stimulations generated by a physical environment have the capacity to produce positive or negative emotional states, depending on the individual’s interpretation of that sensory stimulation.[4] Nursing researcher Patricia Benner and anthropologist Monique Scheer further argue that an individual’s body is central to their communication and performance of emotion, as it is within the body that emotions are registered and through the body that they are conveyed to others.[5]
Scheer builds on Cooper’s argument regarding the influence of an environment’s physical characteristics on an embodied individual in order to address the influence of that environment’s social characteristics. Scheer argues that an individual’s social environment influences the presentation and perception of that individual’s body just as their physical environment does, thereby creating an embodied individual who is both ‘socially and environmentally contextualised’.[6] As a result of this social contextualisation, all bodily structures and processes are in some way impacted by cultural activity.[7] Scheer’s argument regarding the social contextualisation of the embodied individual integrates the body into the theory of emotional communities. Historian Barbara Rosenwein argues that social communities possess accompanying emotional communities that determine what emotions and emotional displays are socially acceptable.[8] Since emotions are experienced and presented through the physical body, the body is subject to these emotional regulations as well. Scheer does not, however, argue that the influence of this social contextualisation is so strong that it eliminates individual agency. Instead, she argues that social contextualisation only provides the individual with a ‘feel’ for the appropriate emotional response and display and, therefore, it also leaves room for alternative or contrary responses.[9]
Within the context of a wartime society such as Second World War Britain, Scheer’s argument regarding the individual’s ability to resist the pressure of their social contextualisation is complicated by Judith Butler’s theories on subjection and Carol Acton’s work on the impact of war on society. Butler argues that an individual will often conform to social categories that may ‘work in the service of subjection’ when those categories offer them a ‘recognisable and enduring social existence’.[10] Acton argues that both the pressure to conform to social categories and the risk to an individual’s social existence are heightened during times of war, making the pressure and the desire to conform to community expectations stronger than under normal circumstances.[11]
A key element to consider when analysing embodied experiences contained within diaries and letters is how those experiences were conveyed via the written word. Historian Catherine Baker and International Relations scholar Synne Dyvik both argue that communicating an embodied experience is an act of translation.[12] An individual must attempt to transform a sensation rooted in the body into a narrative or description that can be understood by another who may not have experienced the same embodied sensation. Dyvik also argues that individuals draw on the discourse of their social and cultural environment in order to make sense of, and coherently communicate, their embodied experiences.[13] Both Scheer and historian Peter Burke have highlighted the importance of language in the understanding and communication of emotion, with Scheer arguing that the ability to put a name ‘on our feelings is part and parcel of experiencing them’.[14] Given the reliance of language on the meanings provided by its social and cultural context, social contextualisation once again comes to the fore as a significant influence on embodied experience. This critical relationship between social discourse and language also means that, should an individual’s embodied experience fall outside of the framework provided by their community, they may struggle to make sense of that experience to themselves and to communicate it to others.
Popular expectations regarding the nurse’s body
Reform nursing placed a high degree of emphasis on the bodily presentation of a professional nurse. Historians of nursing Jane Brooks and Anne-Marie Rafferty have argued that the uniform of the ‘Reformed Nurse’ served as an ‘invented tradition’ that physically represented and enforced the stated values of the profession.[15] With its intentional reference to religious habits, the uniform of the ‘Reformed Nurse’ was intended to provide a commentary on her moral character and project an aura of ‘non-sexual femininity’.[16] However, the visual language of the nurse’s uniform only worked if it was presented in a neat and clean manner. A nurse’s appearance provided a commentary on her professionalism and, within popular understanding, a nurse with an untidy or dirty appearance was understood to be a subpar practitioner.[17]
In addition to an ordered physical appearance, a nurse was also expected to present an ordered emotional display. The 1937 edition of A General Textbook of Nursing stated that a nurse’s role was to produce an environment that was ‘free from fear, inspires confidence and provides an atmosphere of peace, serenity and security’.[18] To do so, her own emotional display must be calm, kind, and cheerfully controlled. In an August 1935 article, the editors of the British Journal of Nursing (BJN) described a ‘satisfactory nurse’ as one who is ‘faithful to duty, kind to her patients, eager and energetic in doing all that she can to better the conditions of people’.[19] In March 1935, another BJN article emphasised the connection between a nurse’s emotional display and patient well being, stating that a nurse’s ‘faltering may incite fear. Her calmness brings hope’.[20] Even prior to the advent of war, social expectations regarding the nurse’s bodily presentation stipulated that a good nurse would maintain her emotional control even in adverse circumstances. In the February 1935 edition of the BJN, the editors praised the nurses of the City of London Institution for their ‘courage, coolness and superb discipline’ while evacuating their patients due to a fire in the building, noting that they undertook the entire process ‘[q]uietly and calmly’.[21] The article concluded its celebration of these nurses’ emotional restraint by thanking them for upholding the nursing profession’s ‘best traditions’.[22] In many cases, calmness alone did not meet the social expectations regarding a nurse’s outward emotional display. A nurse must not only be calm and controlled, but cheerful too. In many ways, the bodily presentation expected of the pre-war British nurse was encapsulated in two Ovaltine adverts placed in the BJN in 1935. The nurse depicted in both adverts was young, pretty, and smiling, dressed in either her tidy uniform or in appropriate outerwear, complete with hat and gloves. Both adverts emphasised the importance of the nurse’s physical and emotional stamina. One stated that ‘Every Nurse knows how much depends upon her own fitness and cheerfulness in all the difficult conditions she may meet’.[23] The other reminded readers that ‘a Nurse must answer the call of duty. It is essential, too, that she should be fit, vigorous and cheerful under the most adverse conditions’.[24] While both adverts directly referred to the adverse circumstances under which nurses work, such circumstances were not depicted as having an impact on the physical display of the nurses, who remained clean, attractive and smiling.
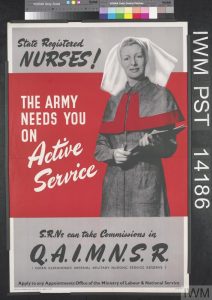
In many ways, with the onset of the Second World War, expectations of the bodily presentation of nurses extended to all British civilians. In an effort to address the problem of civilian morale, Government propaganda encouraged civilians to adopt an outlook of cheerful fortitude, similar to that expected of British combatants.[25] This message was adopted and further propagated by British popular media.[26] In addition to a cheerful outlook, British women were also heavily encouraged to maintain an attractive physical appearance; preserving one’s physical attractiveness was presented as a form of feminine patriotism as a British woman’s beauty could serve as a source of morale for British fighting men. Throughout the war, women’s magazines were filled with adverts and columns exhorting women to maintain their appearance. An advert for cosmetic company, Yardley, encouraged readers to ‘face the future bravely and honour the subtle bond between good looks and good morale’.[27] In a wartime magazine article, actress Ruby Miller argued that it was a woman’s ‘job to bring colour and cheerfulness to the grim business of war’ and that, by maintaining her appearance, she could act as a ‘tonic’ to men on active service. Miller went on to directly associate the maintenance of one’s physical appearance with the war effort, encouraging her readers to be ‘as attractive as you can at work and in leisure hours, and you’ll soon discover what a delightful impression you make on friends and how formidable you can be – indirectly – to foes!’.[28] While pre-war British nurses had been encouraged to maintain a clean and neat appearance, they were now expected to maintain a beautiful appearance as well. In early 1940, nurses were directly referenced in a series of adverts produced by Icilma Beauty Aids. At the top of the advert was a depiction of a beautiful nurse, neatly outfitted in her uniform. Just below this image came the headline for the advert, which read ‘BEAUTY IS YOUR DUTY’. The main body of the text informed readers that ‘Beauty inspires happiness and cheerfulness both for yourself and others’ and celebrated Iclima’s products’ ability to make it ‘possible for thousands of women to do their essential duty of being beautiful’. This was followed by an image of the nurse from the top of the advert, off-duty, wearing a beautiful evening gown, and dancing with a member of the armed forces.[29] In this way, the visual language of the advert argued that the woman’s work as a nurse and her ‘work’ as a social companion for a British combatant both represented ‘essential’ war work. In many ways, the discourse found in this advert and others like it created a paradigm wherein a woman’s appearance offered commentary on her patriotism and her support of the war effort. As a result of this social contextualisation, British nurses entering military service found themselves confronted by an environment where their bodily presentation took on profound significance. The pressure on active-duty QA’s to meet the expectations of this environment was most likely intensified by the fact that they were often the only women British combatants encountered for months and the only British women they encountered for years. Under these circumstances, the QA’s examined here tended to address their embodied engagement with their environment in two ways. They either discussed their body as a tool to be used, or as an obstacle, whose interactions with its environment produced undesirable responses that needed to be silenced or overcome.
The body as a tool
During the Second World War, QA’s often drew on their bodies as tools in their nursing practice, either utilising them as a site of embodied knowledge or as a means of invoking particular emotions in others. Contemporary nursing researchers, such as Patricia Benner, argue for the importance of integrating an understanding and appreciation of the value of embodied awareness in modern nursing practice. Benner argues that it is a nurse’s embodied awareness and knowledge that fuels her intuition regarding her patients, enabling her to pick up on subtle changes in a patient’s status.[30] Furthermore, it is her own embodied awareness that allows a nurse to accurately read her patient’s emotions and respond appropriately.[31] Laura Middleton-Green argues that a nurse’s embodied awareness is especially important in her provision of palliative care. Middleton-Green posits that the embodied awareness of another’s suffering can serve as a source of insight into a patient’s condition, enhancing empathy and the provision of compassionate care.[32]
The nurse’s body as a site of embodied knowledge
Of course, QA’s would not have used terms like ‘embodied knowledge’ to describe their use of their embodied awareness and it is important to guard against presentism in historical analysis. However, the use of this type of knowledge can be found throughout their personal narratives. A key example can be seen in the QA’s use of their sense of smell. Smell often aided in the early diagnosis of infections such as gas gangrene and diphtheria. Sister Mary Morris touched on her use of smell in the detection of gas gangrene twice in her diary. In her entry for 26 June 1944, she wrote, ‘Yesterday’s operation cases are doing fine. They are very cheerful, no signs of gangrene so far. The first sign is smell and we are constantly alert to this’.[33] On 10 February 1945, she once again commented that ‘Smells are important. It is vital to be able to smell the early stages of gangrene as this could mean an emergency amputation’.[34] While in charge of an Isolation block in 1945, Morris acknowledged her use of smell in the diagnosis of diphtheria, writing ‘Fortunately diphtheria has a distinctive smell and appearance’ that allowed her to quickly isolate possible diphtheria patients.[35] Morris needed to rely on her embodied knowledge to inform her diagnosis because the throat swabs that would confirm diphtheria took forty-eight hours to be processed. While Sister Joyce Ffoulkes Parry did not specify which conditions she used her sense of smell to address, she did confirm its importance in her nursing practice in her diary entry of 28 November 1940 where she described her relief at coming off of night duty: ‘It is so marvellous to come off in the morning and to know that you have got two whole nights to yourself and that the ward with its smells and worries – these in the correct order as to their importance please note – may be temporarily forgotten.’[36]
Ffoulkes Parry’s insistence that she had placed smells and worries in the correct order according to importance appears to allude to Morris’s belief that smell served as a key warning sign in their nursing practice. Given the importance of smell in detection and diagnosis, it was critical that a nurse be present and aware of her embodied experience. She could not disassociate from the sensory world around her without potentially placing her patients at risk.
Another key example of the QA’s use of embodied knowledge was in their approach to pain management. During the Second World War, British combatants were expected to face their pain stoically and without complaint. Nurses, therefore, had to draw on their embodied knowledge to determine when to administer their patients’ pain medication as the patients themselves often would not ask for it.[37] Sister Betty Murgatroyd referred to this use of embodied knowledge in a 1944 letter to her friend, Lilian Church. ‘[My] patients never bat an eye lid, and always are quite OK if you ask. They never ask for anything, and if I did not sense their wants, they would never ask.’[38] This use of embodied knowledge was even visible to outsiders as a journalist was able to capture its deployment in an article describing a senior sister caring for a captured German general.
The General himself was in great pain, but he lay without making a sound. The Sister who sat beside him did not make the mistake of appearing to notice this. She knew better than to offer sympathy or ask irritating questions of one of his breed. … After a few moments he added, “You nursed the men of our Old Army? The Old Army was very different from the new – “ She got up quietly and gave him his medicine.[39]
It is unclear if the em dash at the end of the General’s sentence was meant to imply that he was cut off by pain or if it was a stylistic decision made by the author. However, the author does make clear the nuanced process that the nurse employed in her treatment of this patient. She needed to draw on her embodied knowledge to both read her patient’s emotions, allowing her to determine that sympathy and acknowledgement of his pain would not be welcome, and to ‘sense’ when his pain had moved past the point where she could allow him to suffer through it. Once that point had been reached she could provide him with pain medication without simultaneously insulting him.
The nurse’s body as a source of emotional comfort
Second World War military leaders made the decision to post QA’s further forward than they had in previous conflicts. There were two reasons behind this change: the first was the expert nursing care that the QA’s could offer and the second was the psychological benefit that their presence, as women, provided male combatants. Cultural assumptions regarding the innate caring nature of women meant that combatants often believed that a female nurse would be naturally kind and understanding and that the care she offered would be more compassionate and skilled than that offered by male Royal Army Medical Corps (RAMC) orderlies. This mentality can be seen in a letter sent from a British Colonel deployed to the Anzio beachhead.
God bless ‘em, the QA’s are here! Our own women are with us … Now this does not one whit detract from our men of the RAMC. I have been touched almost to tears at the tenderness of a man to a man, but the QA’s bring more than tenderness. No more strategically intelligent order was ever given as when the QA’s were sent to the beach head …[40]
While this Colonel insists that RAMC orderlies were capable of exceptional care, he still believed that the care offered by female QA’s was superior. A letter from Matron Thorp (of the 16th British General Hospital) to the Matron-in-Chief, Dame Katherine Jones, also noted patients’ association between QA’s and superior care. She wrote that the ‘men were so grateful to see Sisters. I remember one night when a large number of wounded men were brought in hearing a man say to another who was also very badly wounded – “We shall be all right here, there are Sisters”’.[41] The QA’s drew on these positive associations in order to use their physical presence as a source of comfort for their patients. This can be seen in their descriptions of sitting and talking with their patients, holding their hands, or simply being visible to them. In a February 1943 letter to her mother, Sister Agnes Morgan recounted her experiences with a very ill patient, who was ‘going through a stage of “wandering” in which he gets very frightened’.
Morgan used her physical presence to comfort him by spending ‘a good part of every night with him’ holding his hand.[42] Similarly, Sister Ffoulkes Parry recounted using her physical presence to comfort a patient by sitting with him throughout an air raid. The patient in question had been a survivor on two different ships that had been sunk by aerial bombardment and Ffoulkes Parry wrote that she knew how much air raids ‘unnerve him’. The comfort that this patient derived from her presence can be seen in the note he sent her, which read ‘Sister, you were awfully sweet to me, early this morning. Thanks a lot’.[43] QA’s drew on the assumptions connected with their gender in order to use their physical presence to not only provide their patients with a sense of comfort and physical safety, but to also invoke a sense of emotional safety that allowed their patients to psychologically unburden themselves. QA’s frequently commented on the time that they spent listening to their patients talk about their experiences. On 12 December 1940 Ffoulkes Parry noted in her diary that she had sat with a patient who had just learned that his parents had been killed in an air raid.
Poor Morris, no one had been near him all day – I suppose they would feel that he wanted to get away – but he did want to talk about it and go over and over it. I felt that he did so I went to sit on his bed, which I imagine is still verboten, and stayed with him for a very long time.[44]
Ffoulkes Parry appeared to draw on her embodied awareness in order to read Morris’ emotions and determine what action she should take, as evidenced by her statement that she ‘felt’ that he would want to talk about his loss. In her entry, Ffoulkes Parry did not mention if she made any verbal overture to Morris to invite him to speak with her about his feelings. Instead, she highlighted the physical act of sitting beside him and staying with him, drawing attention to the comfort that was derived from her physical presence rather than her words. Similarly, Sister Mary Morris’ diary entries following the failed British attack on Arnhem were filled with her patients’ accounts of their traumatic experiences. On 6 October 1944, Morris wrote that the ‘Arnhem boys were still talking about their shocking experiences when I went on duty this morning. They were delighted to see me, someone to listen to them at last. They talk and talk and I encourage them to do so’.[45] The comfort that these men derived from the physical presence of a woman can be seen in the fact that, when they could not confide in Morris, they turned to a Belgian nun named Soeur Marie-Anselma, who assisted Morris on the ward. Although Marie-Anselma could not speak English, Morris wrote that she looked ‘so sympathetic and understanding’ that her patients did ‘not know or care’ that she couldn’t understand them.[46] Morris’ patients’ decision to confide in Marie-Anselma does not appear to be the result of having no other alternative if Morris herself was not available. Morris was also assisted on her ward by at least one RAMC orderly, a Welsh man named Taffy Jones. Morris does not record her patients engaging in similar conversations with Jones: the comfort that Marie-Anselma’s physical presence as a woman offered appears to have been more valuable to these patients than Jones’ ability to understand them.

The QA’s had the ability to amplify the psychological benefit derived from the presence of a woman by virtue of being British women, serving as an embodied connection to combatants’ homes. Many QA’s commented on the pleasure combatants expressed on encountering British women overseas. Sister Vera Jones wrote to her parents of her experience nursing a fellow Essex native, explaining that ‘These lads love to meet someone who knows their own county’.[47] In a June 1943 letter, Sister Morgan recounted a tea dance she attended with members of the 8th Army and stated ‘DO you know what I was told at least six times? And with perfect truth I know, “This is the best afternoon I’ve spent for TWO YEARS, Sister!” and many and many another said, “You’re the first English girl I’ve spoken to for eighteen months!”’[48] In an undated letter sent several months later, Morgan described soldiers’ responses to seeing nurses pass by their camps and commented that her mother had ‘no idea, and cannot imagine the feelings these poor, lonely, grubby, weary boys have for us and the welcome they always give us when they see us following on behind their lines’.[49] A key factor in the QA’s ability to produce this positive response from British combatants was their ability to present attractive British womanhood. Sister Murgatroyd wrote of British soldiers’ positive response to the arrival of ‘real English girls’ in Normandy, ‘complete with lipstick on’.[50] Upon receiving British patients from a captured German hospital, Sister Morris noted that their primary ‘complaint’ about their treatment was that ‘the Germans did not have pretty nurses like us!’[51] Morgan acknowledged the expectation for attractiveness in an early letter home in which she wrote that ‘we were expected (and somehow we managed it) to look as though we’d come straight out of a band box at all hours of the day and night under all circumstances’.[52] This statement followed Morgan’s account of having to change her blouse five times before feeling that she could attend the church service aboard her troopship because the heat was so severe she kept sweating through her blouses.[53] Clearly, even early on in a QA’s deployment, meeting this expectation for attractiveness was not an easy endeavour.
The nurse’s body as an obstacle
During the Second World War, QA’s were expected to embody the image of a clean, attractive and cheerful British woman. However, the conditions within which they worked often created an embodied experience that made it difficult for QA’s to consistently achieve that desired bodily presentation. Under these circumstances, their bodies shifted from tools to be used in their nursing practice to obstacles, whose response to negative embodied experiences had to be overcome. The factors that appeared to most frequently hinder the QA’s ability to present this expected embodied performance were exhaustion, negative sensory experiences and illness.
While the QA’s training and time in civilian hospitals had often been characterised by long hours and hard work, nursing on active service took these demands to new heights through the scale of the work required and the rapidity with which it could escalate.[54] In her entries written during the German invasion of France in 1940, Sister Helen Luker described working in her unit’s operating theatre for over seventeen hours.[55] Four years later, during the Allied invasion of Normandy, Sister Murgatroyd wrote of spending thirty-six hours on duty, sleeping for three hours, and then returning to her ward.[56] The exhaustion generated by their workload impacted the QA’s physical and emotional experience and in turn influenced their external physical and emotional display. In their diaries and letters, the QA’s ruminated on their sore backs and feet and the burdensome sensation of their physical exhaustion.[57] They also acknowledged the emotional impact that exhaustion had on them. In May 1942, Sister Morgan wrote in a letter of ‘devastating homesickness’ which she credited to her exhaustion from spending seven weeks on night duty.[58] In her diary entry for 3 October 1942, Sister Luker described her abortive attempts to sleep during the day before going on night duty, writing ‘No sleep all the afternoon till 4pm then emergency stations at 4:30 — !’.[59] Luker often used an em dash followed by an exclamation point as shorthand for her anger and frustration, letting those two punctuation marks imply all the incensed comments that she might have otherwise said. Sister Ffoulkes Parry noted how her exhaustion emotionally deadened her to experience of saying goodbye to her close friend, writing that ‘I ought to feel this moment more’.[60]

Wartime nursing also exposed the QA’s to more extreme sensory experiences. QA’s deployed to North Africa, the Middle East and India reported working in temperatures ranging from 35 to 49℃. Sister Luker described the physical and emotional impact of this extreme heat, writing ‘we’re nearly expiring. Sim is off sick with ? heat stroke, and we’re all feeling pretty grim’.[61] From her field hospital in Libya, Sister Morgan wrote that by ’10 o’clock life is a bit of a burden, by noon we are thoroughly out of humour’.[62] In addition to the heat, QA’s in North Africa and the Middle East often had to deal with sandstorms, which, outside of the negative sensory experiences these events caused them personally, added to their workload by making the maintenance of an aseptic environment nearly impossible.[63] In contrast to this, QA’s in Europe and India often commented on the difficulties created by mud while working in tented hospitals and the effort required to keep it out of their wards and sleeping quarters. In a 22 July 1944 letter, Sister Murgatroyd recounted heavy rains flooding one of her wards with three inches of water, leaving her with ‘mud simply up to my knees’. Murgatroyd then described going off duty only to find that the rain had gotten into her tent and soaked her bed, driving her to sleep on the ground.[64]
In addition to exposing the QA’s to extreme physical environments, the war also amplified many of the negative sensory elements of nursing care itself. In their civilian lives, the QA’s had dealt with injuries, bodily fluids and unpleasant odours. The war took these negative sensory experiences to new extremes. The QA’s often found themselves confronted with patients with extensive physical trauma and levels of infection that they had never seen before. While stationed in Normandy, Sister Morris described caring for burn victims whose appearance she found ‘horrific’.[65] In an entry recounting her hospital’s admission of casualties from the North African campaign, Sister Luker, a senior and experienced nurse, wrote that ‘Some of the officers have ghastly wounds, the smell and crawling – ’.[66] Luker’s inability to finish her description, cutting off her sentence with a dash, indicates the level of distress this experience caused her. Much like nurses today confronted with patient conditions that trigger a negative visceral response, QA’s had to consciously work to suppress and hide those reactions from their patients. The pressure placed upon Second World War QA’s to conceal these reactions was especially strong. A QA’s response to a soldier’s injury could be seen as a precursor to their loved ones’ response and that of civil society as a whole.
The greatest obstacle that a nurse’s body could create was succumbing to illness. All of the nurses examined here struggled with illness over the course of their deployment. These illnesses ranged from persistent ear infections to life threatening conditions such as amoebic hepatitis. The experience of falling ill far from home in a strange environment was both physically and emotionally draining. However, in the personal narratives examined here, a key element in the emotional impact of illness appears to be that it prevented the QA’s from working. British nursing culture was profoundly impacted by notions of vocationalism and self-sacrifice and it was a common expectation that nurses would consistently place patient needs above their own.[67] Articles published in the BJN describe nursing as ‘creative service’, argued that the ‘real depth of nursing can only be made known through ideals, love, sympathy, knowledge and culture’ and that ‘Many Registered Nurses are feeling to-day that the great need to their profession is to re-capture the spirit of devotion to the sick which inspired Religious Sisters for centuries’.[68] The impact of this expectation can be seen in the fact that almost all of the QA’s examined here continued to work while ill and often only stopped working when they were physically incapable of continuing or were ordered off the ward by a superior. Illness went farther than any other negative sensory experience to impede a QA’s ability to provide the embodied presence required of her by removing her body from the ward entirely.
Finding the right words: narrating an embodied experience
Thus far this article has focused on the specific elements of the QA’s embodied experience that they chose to highlight in their personal narratives. It will now turn its attention to how they set about narrating these experiences. In their narration of the times when they used their bodies as tools, QA’s directed their attention outside of themselves and towards their patients. Notably, discussions of the use of smell in clinical practice were accompanied by very little descriptive or emotive language. The scent of gas gangrene or diphtheria was not pleasant but this fact was not directly acknowledged in the QA’s diaries or letters. The closest admission to the unpleasant nature of this embodied experience can be found in Ffoulkes Parry’s statement that she was relieved to leave the smells of her ward behind.[69] In general, QA’s narrated their experiences of using their bodies as tools in their practice in relatively simple value-neutral or positive manners. They particularly emphasised the pleasure they received from the sense that they were bringing their patients’ comfort and that their work was of use. For example, following her discussion of her ability to ‘sense’ her patients’ needs, Sister Murgatroyd simply stated ‘how honoured, and proud I am to be able to do a little to help them’.[70]
The QA’s narrative strategies for capturing negative embodied experiences were more complex. Detailed and emotive descriptions of their experiences confronting negative embodied sensations were rare and oftentimes their most strident accounts were focused on the impact that a negative sensory experience had on their patients. Morgan was the most descriptive writer of the QA’s examined here and her account of the experience of nursing in a desert field hospital was particularly harrowing.
Sometimes after a particularly wearying day, when one’s heaved and pulled and pushed and shifted the beds and made room for more and more and more and tried and tried again with almost nothing to bring a bit of comfort to the endless stream of bearded heroes in all states and conditions, and all the time one’s eyes are running with the blinding glare of the blowing sand and one’s mouth is full of it and you want to stand still in the middle of this bedlam and say “Oh, if only everything would keep still for 1 minute, if the wind would stop and the sand would stop and the canvas would stop flapping and we could have 1 minute’s respite in which to collect our thoughts!!!”[71]
Morgan’s use of repetition and her decision to not break her account up into separate sentences helps to convey the chaotic and overwhelming nature of her embodied experience. However, it is important to note that she prefaced this portion of her letter with her musings on what she deemed to be the more ‘difficult’ embodied experience of British combatants, writing ‘how these marvellous men fight on and on thro’ these frightful conditions I don’t know’.[72] Furthermore, a key element feeding her distress was the impact that this embodied experience had on her ability to bring comfort to her patients. Similarly, while stationed aboard a hospital ship operating in the Red Sea, Luker described the negative impact of extreme heat in the wards, writing that it was ‘like an oven, filthy and quite unfit for any sick people – its too disheartening for words and I feel ready to weep’.[73] Ffoulkes Parry’s account of her time on a hospital ship in the same area in many ways echoed Luker’s.
But the chief remembrance of Massawa for all of us will simply be the heat. It seems there are degrees of heat, even of extreme heat, and that was the superlative of them all … The poor patients, disgracefully overcrowded, simply queued up for air under the few fans which were available … It would do British Army Incorporated the world of good to spend one whole night in C Ward for a change just to see how they would enjoy it. It is a sheer disgrace. I was called to supervise two epileptic fits and I felt it would be a good thing if I had had one myself … We drink and drink – gallons – and then we drip and drip until our skins are sore with mopping.[74]
Like Morgan, both Luker’s and Ffoulkes Parry’s narrations of their negative embodied experiences were structured by their impact on their patients. In the instances when the QA’s directly addressed the negative sensory elements of living and working in extreme heat without focusing on their patients, they often highlighted the aspects of that embodied experience that made them appear less attractive or pulled together. While in the Red Sea, Luker lamented that she was ‘literally saturated from my head to my heels – my stockings are sodden – so disgusting!’[75] Sister Nell Jarrett characterised her time in Aden as consisting of ‘much indecent looking sweating’ and Sister Jones noted that the heat rash she and her colleagues contracted in Secunderabad, India, ‘fortunately does not affect the face, or one would look a mess!’[76] This focus on the impact of heat on their appearance supports the argument that the pressure to embody the image of attractive British womanhood influenced the way these QA’s perceived their embodied experience.
In their discussions of their embodied experiences, QA’s most frequently used a narrative strategy that consisted of a pattern of revelation accompanied by subsequent concealment or dismissal. QA’s concealed the negative elements of their embodied experience by framing them with either humorous or minimising language or by diminishing their severity by contrasting them with an embodied experience that was ‘worse’. For example, while Luker admitted that the heat in the Red Sea left her feeling like she was ‘nearly expiring’, she then undercut her narrative by using a minimising modifier (‘pretty’) to describe her emotional state (‘pretty grim’).[77] Similarly, Jones informed her parents that it was ‘very hot indeed here now, the temperature ranges between 110 and 112 degrees F’ and then promptly minimised her own complaint by stating that ‘of course we are lucky really as it is not as hot as some places’.[78] Murgatroyd confided in her friend Lilian about the negative emotional impact of her continually cold living quarters only to quickly dismiss her experience by writing ‘it’s beastly of me to complain I know … when some of our poor boys are continuously up to their middles in water’.[79] Morgan concluded her description of working in the heat of a field hospital in Libya with a cheerful account of swimming in the Mediterranean and attending dances in the evening, writing that she hoped her mother had found her story amusing.[80] Murgatroyd also turned her account of nursing in a flooded ward into an amusing anecdote, assuring Lilian that ‘once I got all the boys onto the boxes, we had many laughs’.[81]
This narrative strategy was especially common in the QA’s accounts of falling ill. Sister Jones only informed her family that she had contracted hepatitis after she had recovered and she spent the majority of the letter describing her illness, joking about how yellow her jaundice had made her.[82] In a June 1943 letter recounting her experience of being hospitalised with dysentery, Morgan adopted a similarly cheerful and jocular tone and focused on the hospital’s pleasant amenities, writing that since her admission she had ‘lived a life of ease – oh! and dysentery, I nearly forgot that!’[83] While Luker’s entries recording her battle with a bout of amoebic hepatitis that nearly killed her did not take on a cheerful tone, her language was still restrained. In the last two entries before an extended break that marked the height of her illness, Luker’s strongest statements regarding her embodied experience were that she was ‘most uncomfortable’ and ‘not feeling at all well’.[84] It was only in a retrospective account that Luker described her embodied experience at this time as ‘agonizing’.[85]
Conclusion
In her 1943 Nursing Times article, Dame Katherine recounted the story of a QA going to administer care to a severely wounded officer while under machine gun fire. Dame Katherine informed her readers that, based on her personal knowledge of this particular nurse, she was certain that this QA would not view her act as one of extreme bravery. Rather, she insisted that this QA would simply state that ‘she “forgot about herself”’.[86] In many ways, this was the task that was asked of all QA’s, to forget about themselves. Yet both the highly adverse environments in which they worked and the importance of their embodied awareness to their nursing practice made such forgetting impossible. QA’s could not avoid comprehending their embodied experience. This paradoxical position fostered an ambivalent relationship between QA’s and their bodies and informed the ambiguous narrative strategies that they used to describe their embodied experiences. A more in-depth understanding of the QA’s relationship with their own embodiment helps to highlight the profound emotional pressures under which these women lived and worked, thereby adding a more nuanced perspective to the history of nursing during the Second World War.
References
[1] Katherine Jones, ‘On Active Service with the Army’, Nursing Times, 25 September 1943, 719.
[2] A central aim of Merleau-Ponty’s philosophy was the cessation of a dualistic approach to experience that considered the mind and body as separate entities. Merleau-Ponty held that mind and body were united into one embodied being. Helen F. Harrison, Elizabeth Anne Kinsella, and Sandra DeLuca. ‘Locating the Lived Body in Client–Nurse Interactions: Embodiment, Intersubjectivity and Intercorporeality’, Nursing Philosophy 20/2 (2019), e12241, 4, 6. Referencing Maurice Merleau-Ponty, Phenomenology of Perception, (New York: Routledge, 2012).
[3] Harrison, Kinsella, and DeLuca, ‘Locating the Lived Body’, 5.
[4] Rachel Cooper, ‘Wellbeing and the Environment: An Overview’, in Wellbeing and the Environment, ed. by Rachel Cooper, Elizabeth Burton and Cary L. Cooper (Chichester: John Wiley & Sons, 2014), 2.
[5] Patricia Benner, ‘The Roles of Embodiment, Emotion and Lifeworld for Rationality and Agency in Nursing Practice’, Nursing Philosophy 1/1 (2000), 11; Monique Scheer, ‘Are Emotions a Kind of Practice (and Is That What Makes Them Have a History)? A Bourdieuian Approach to Understanding Emotion’, History and Theory 51/2 (2012), 193-4.
[6] Scheer, ‘Are Emotions a Kind of Practice’, 197.
[7] Ibid., 201.
[8] Barbara H. Rosenwein, ‘Worrying about Emotions in History.’ The American Historical Review 107/3 (2002), 842.
[9] Rosenwein, ‘Worrying about Emotions in History’, 204.
[10] Carol Acton, Grief in Wartime: Private Pain, Public Discourse (Basingstoke and New York: Palgrave Macmillan, 2007), 4.
[11] Acton, Grief in Wartime, 4-5.
[12] Catherine Baker, ‘Writing about Embodiment as an Act of Translation’, Critical Military Studies 2/1–2 (2016), 120; Synne L. Dyvik, ‘Of Bats and Bodies: Methods for Reading and Writing Embodiment’, Critical Military Studies 2/1–2 (2016), 61.
[13] Dyvik, ‘Of Bats and Bodies’, 62.
[14] Scheer, ‘Are Emotions a Kind of Practice’, 212; Peter Burke, ‘Is There a Cultural History of the Emotions?’, in Representing Emotions: New Connections in the Histories of Art, Music and Medicine, ed. by Penelope Gouk and Helen Hills (Aldershot: Ashgate, 2005), 43.
[15] Jane Brooks and Anne Marie Rafferty, ‘Dress and Distinction in Nursing, 1860–1939: “A Corporate (as Well as Corporeal) Armour of Probity and Purity”’, Women’s History Review 16/1 (2007), 44.
[16] Brooks and Rafferty, ‘Dress and Distinction’, 42.
[17] Ibid., 47.
[18] Evelyn Peace, A General Textbook of Nursing: A Comprehensive Guide to the Final State Examinations (London: Faber & Faber, 1937), 2. As quoted in Jane Brooks, ‘“Not Only with Thy Hands, But Also with Thy Minds”: Salvaging Psychologically Damaged Soldiers in the Second World War’, Nursing History Review 27 (2019), 41.
[19] ‘Nursing Echoes’, The British Journal of Nursing, August 1935, 200. All BJN content was accessed via the British Library.
[20] E. Marguerite Gane, ‘What the Social Worker Expects of the Nurse’, The British Journal of Nursing, March 1935, 65.
[21] ‘Nursing Echoes’, The British Journal of Nursing, February 1935, 32.
[22] Ibid., 32.
[23] ‘I Rely on OVALTINE to Keep Fit and Cheerful’, The British Journal of Nursing, August 1935, iv.
[24] ‘When the Weather’s at Its Worst “OVALTINE” Is Your Best Safeguard of Health’, The British Journal of Nursing, December 1935, iv.
[25] Patricia Jalland, ‘A Culture of Silent Grief: The Transformation of Bereavement Care in 20th Century England’, Bereavement Care 32/1 (2013), 18.
[26] Jane Waller and Michael Vaughan-Rees, Women in Wartime: The Role of Women’s Magazines 1939-1945. (London: Macdonald Optima, 1987), 32.
[27] Waller and Vaughan-Rees, Women in Wartime, 104.
[28] Ruby Miller, ‘Don’t Get Slack!’, as reproduced in Waller and Vaughan-Rees. Women in Wartime, 81.
[29] Waller and Vaughan-Rees, Women in Wartime, 100.
[30] Benner, ‘The Roles of Embodiment’, 7.
[31] Ibid., 12.
[32] Laura Middleton-Green, ‘Nursing Intuition: The Role of Embodied Awareness in End-of-Life Care’, International Journal of Palliative Nursing 21/6 (2015), 265.
[33] Mary Morris, A Very Private Diary: A Nurse in Wartime, ed. by Carol Acton (London: Weidenfeld & Nicolson, 2014), 119.
[34] Morris, A Very Private Diary, 181.
[35] Ibid., 252.
[36] Joyce Ffoulkes Parry, Joyce’s War: The Second World War Journal of a Queen Alexandra Nurse, ed. by Rhiannon Evans (Stroud: The History Press, 2015), 61.
[37] Jane Brooks, Negotiating Nursing: British Army Sisters and Soldiers in the Second World War (Manchester: University Press, 2018), 43.
[38] B. Murgatroyd, ‘Private Papers of Miss B. Murgatroyd’, Imperial War Museum, Documents 19944, 24 June 1944, 6-7.
[39] Elizabeth Kyle, ‘Hospital in the Desert’, QARANC Museum, Box 18, 69.
[40] ‘Extract from letter to his wife from Col. – while returning from Anzio Beach Head’, Dame Katherine Jones’ Papers, Envelope 3: Letters and Reports, Museum of Military Medicine.
[41] ‘Extracts from Letters’, Dame Katherine Jones’ Papers, Envelope 3: Letters and Reports, Museum of Military Medicine.
[42] Agnes Kathleen Dunbar Morgan, ‘Private Papers of Miss AKD Morgan’, Imperial War Museum, Documents 16686, 146.
[43] Ffoulkes Parry, Joyce’s War, 86.
[44] Ibid., 64.
[45] Morris, A Very Private Diary, 155.
[46] Ibid., 155.
[47] Vera K. Jones, A Time to Remember: A Record of Nursing Experiences, Impressions, and Travels during World War II Contained in Letters Sent Home from the East (London: Athena Press, 2005), 233.
[48] Morgan, ‘Private Papers’, 186-187.
[49] Ibid., 215-16.
[50] Murgatroyd, ‘Private Papers’, 18 June 1944, 1.
[51] Morris, A Very Private Diary, 131.
[52] Morgan, ‘Private Papers’, 17.
[53] Ibid., 16.
[54] Brooks, Negotiating Nursing, 27.
[55] E.H.A. Luker, ‘Private Papers of Miss EHA Luker’, Imperial War Museum, Documents.1274, 19-20 May 1940.
[56] Murgatroyd, ‘Private Papers’, 22 July 1944, 2.
[57] Luker, ‘Private Papers’, 10 May 1940; Ffoulkes Parry, Joyce’s War, 145; Morris, A Very Private Diary, 29.
[58] Morgan, ‘Private Papers’, 83.
[59] Luker, ‘Private Papers’, 3 October 1942.
[60] Ffoulkes Parry, Joyce’s War, 193.
[61] Luker, ‘Private Papers’, 29 May 1941.
[62] Morgan, ‘Private Papers’, 191.
[63] Jane L. Forrest, ‘Travel with the Q.A.’s – Samaritans in the Near East’, Nursing Times, 22 April 1944, 286.
[64] Murgatroyd, ‘Private Papers’, 22 July 1944, 1-2.
[65] Morris, A Very Private Diary, 129.
[66] Luker, ‘Private Papers’, 18 December 1940.
[67] Deborah Palmer, “‘To Help a Million Sick, You Must Kill a Few Nurses”: Nurses’ Occupational Health, 1890–1914.’ Nursing History Review 20/1 (2012), 36.
[68] Annie Goodrich, ‘Presentation of Certificates by Dean Goodrich: The Address.’ The British Journal of Nursing, July 1935, 177; ‘A Cultural Background’, The British Journal of Nursing, March 1935, 57; ‘Nursing Echoes’, The British Journal of Nursing, October 1935, 256.
[69] Ffoulkes Parry, Joyce’s War, 61.
[70] Murgatroyd, ‘Private Papers’, 24 June 1944, 7.
[71] Morgan, ‘Private Papers’, 93-94.
[72] Ibid., 93.
[73] Luker, ‘Private Papers’, 25 May 1941.
[74] Ffoulkes Parry, Joyce’s War, 162.
[75] Luker, ‘Private Papers’, 28 May 1941.
[76] Nell Jarrett, ‘Diary’, Dr. Jane Brooks’ Private Collection, 20 August 1942; Jones, A Time to Remember, 270.
[77] Luker, ‘Private Papers’, 29 May 1941.
[78] Jones, A Time to Remember, 272. NB: 110 and 112 degrees F is equivalent to 43 to 44 degrees centigrade.
[79] Murgatroyd, ‘Private Papers’, 17 November 1944, 8.
[80] Morgan, ‘Private Papers’, 192.
[81] Murgatroyd, ‘Private Papers’, 30 July 1944, 5.
[82] Jones, A Time to Remember, 191-92.
[83] Morgan, ‘Private Papers’, 182.
[84] Luker, ‘Private Papers’, 4-5 March 1943.
[85] Luker, ‘Private Papers’, 20 March 1943.
[86] Jones, ‘On Active Service with the Army’.
